More than half of younger women’s heart attacks are from nontraditional causes
“These patients often lack traditional cardiovascular risk factors, and as a result, their symptoms may not always trigger a full cardiac workup.”
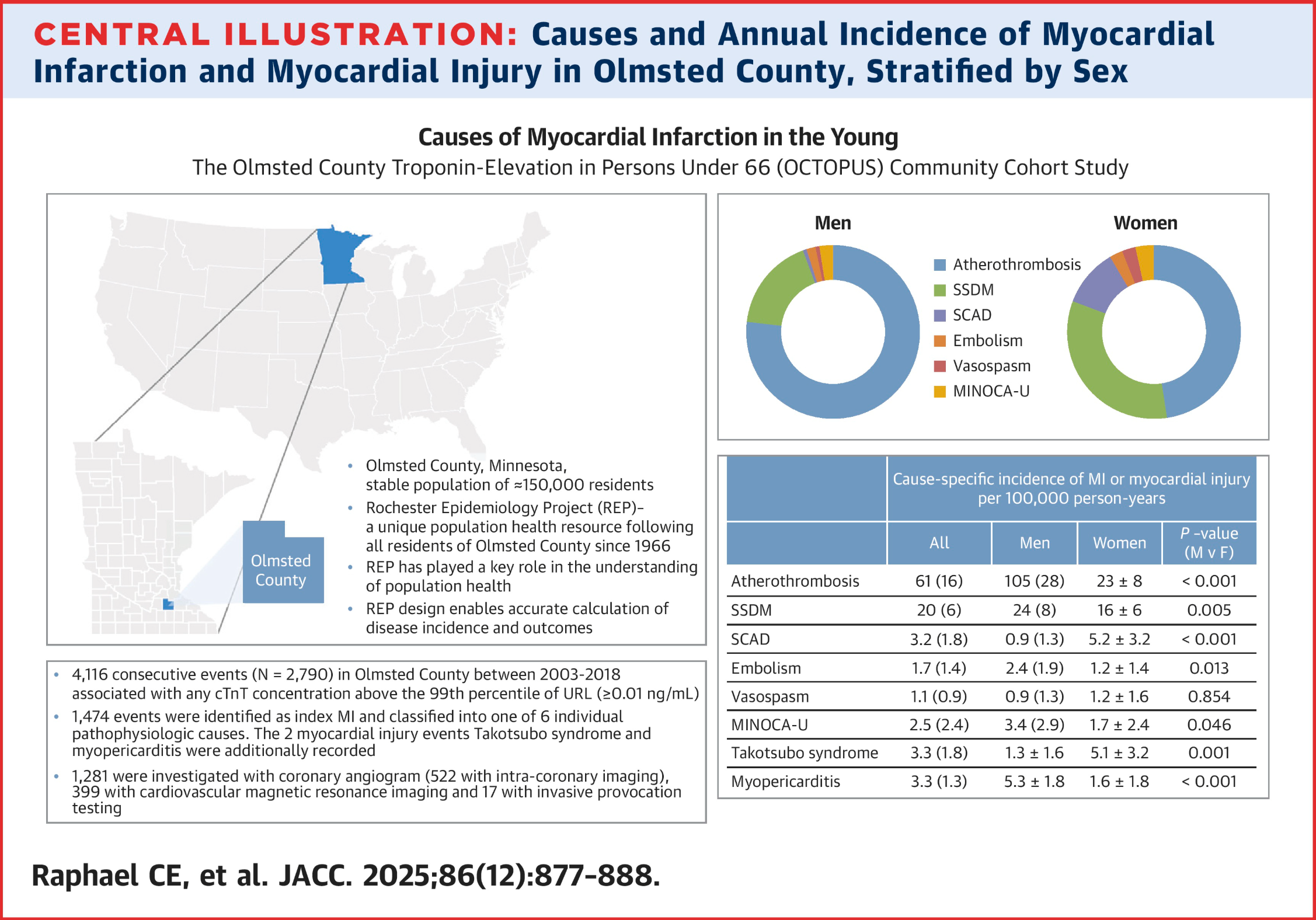
Research recently published in the Journal of the American College of Cardiology that other pathologic mechanisms than atherosclerosis accounted for a large percentage of heart attacks in their study population, even more than half in women less that 65 years old.
“We sought to determine the incidence and outcomes of MI [myocardial infarction - heart attack] according to a unique pathophysiologic mechanism in a large community cohort aged ≤65 years, and to evaluate sex-differences in etiology.”
Atherothrombosis is the term for when a blood clot (thrombus) forms on a ruptured or eroded atherosclerotic plaque (a buildup of fat, cholesterol, and other substances in an artery wall.) There were five causes other than traditional atherothrombosis:
Spontaneous coronary artery dissection (SCAD)
Embolism [obstruction of an artery by a blood clot or bubble]
Vasospasm [spasmodic contraction of the blood vessel]
Myocardial infarction with non-obstructed coronary arteries of unknown cause (MINOCA-U) [unknown]
Supply-demand mismatch (SSDM). [an imbalance where the heart's need for oxygen exceeds the amount supplied by the blood, leading to myocardial ischemia (reduced blood flow to the heart muscle)]. Contributing causes can include hypertension increasing the heart’s workload, tachycardia (rapid heart rate) (e.g., from an arrhythmia), excess physical exertion beyond the individual’s tolerance when a sudden increase in activity raises the heart's oxygen needs; and other conditions including severe anemia, fever, or other systemic illnesses can increase the heart's demand for oxygen.
The data showed a preponderance of other causes for heart attack besides the typical atherothromotic.
“There were 4,116 myocardial injury events in 2,780 patients (36% women) over 15 years. Excluding periprocedural MI [heart attacks occurring during surgery, etc.], 1,474 events were classified as index MI [typcial heart attacks], of which 68% were caused by atherothrombosis [clots]. The population incidence of MI was much lower in women, particularly in MI caused by atherothrombosis (48 vs 137 per 100,000 person years and 23 vs 105 per 100,000 person-years). Incidence of SCAD was much higher in women (3.2 vs 0.9 per 100,000 person-years) with 55% of cases misclassified as MINOCA or atherothrombosis at index presentation. Women with atherothrombosis were similar in age to men (55 ± 8 years vs 54 ± 8 years), with similar disease extent at angiography but greater burden of risk factors. Proportionately, nonatherothrombotic causes comprised the majority of MI in women (atherothrombosis 47% vs 75%, secondary myocardial infarction [SSDM] 34% vs 19%, SCAD 11% vs 0.7%, embolism 2% vs 2%, vasospasm 3% vs 1%, MINOCA-U 3% vs 2%). The 5-year all-cause mortality was highest after SSDM (SSDM 33%, atherothrombosis 8%, embolism 8%, SCAD 0%) with low cardiovascular mortality in all groups.”
Doctors and other providers should to vigilant about these possibilities and willing to dig deeper and more comprehensively into the individual’s risk factors beyond atherosclerosis.
The authors conclude:
“This community-based study demonstrates nonatherothrombotic causes comprise an important burden of acute MI in persons age ≤65 years, particularly women. These cause-specific findings have implications for individualized management and risk stratification and provide epidemiologic benchmarking for future studies.”